In the evolving landscape of healthcare, several persistent challenges continue to hinder optimal care delivery, particularly in integrating mental and physical health services. Fragmented care, limited access to mental health resources, and insufficient coordination among healthcare providers often result in suboptimal outcomes for patients. These issues are further exacerbated by health disparities, especially among racial and ethnic minority populations, who face additional barriers t
o accessing quality care. Addressing these pain points requires innovative, comprehensive solutions that unify different aspects of healthcare to provide holistic, patient-centered care.
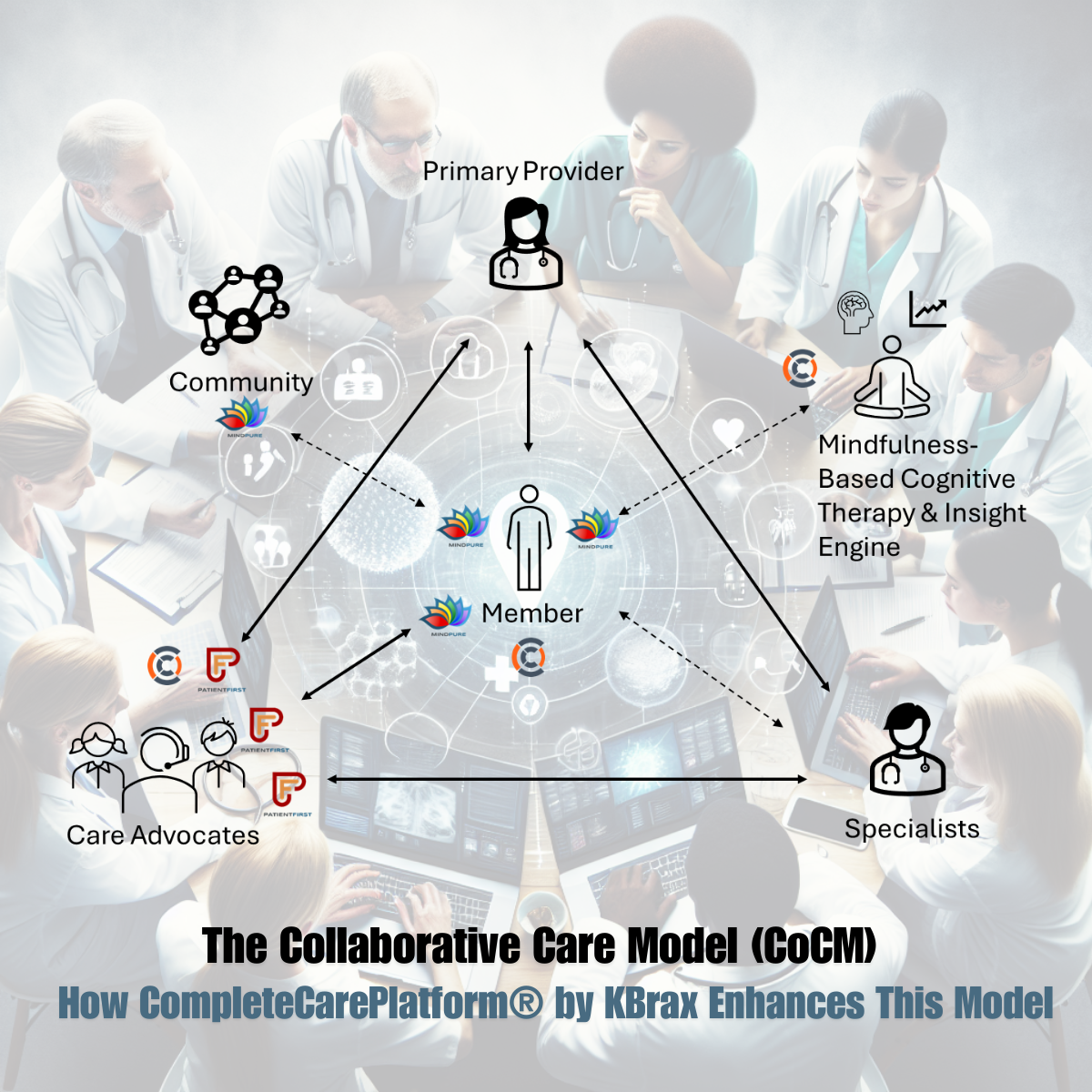
Understanding the Collaborative Care Model (CoCM)
The Collaborative Care Model (CoCM) employs a systematic approach involving a multidisciplinary team of healthcare professionals, each working at the peak of their expertise. This team, led by a primary care provider (PCP), includes behavioral health care managers, psychiatrists, and frequently other mental health professionals. Together, they follow a measurement-driven care plan based on evidence-based guidelines, with special focus on patients who are not achieving their clinical goals.
CoCM distinguishes itself from other integrated behavioral health services through its strong evidence base, consistent adherence to chronic care principles, and a focus on accountability and quality improvement. The five core components of the Collaborative Care Model are:
How It Works
- Patient-Centered Team Care: Primary care and behavioral health providers work together using shared care plans that reflect patient goals. This collaborative approach allows patients to receive both physical and mental health care in a familiar environment, reducing redundant assessments. Enhanced patient engagement often leads to a better healthcare experience and improved outcomes.
- Population-Based Care: The care team oversees a defined group of patients tracked in a registry to ensure comprehensive care. They monitor and reach out to patients who are not showing improvement, with mental health specialists providing focused consultation rather than occasional advice.
- Measurement-Based Treatment to Target: Each patient’s treatment plan outlines clear personal goals and clinical outcomes, which are regularly assessed using evidence-based tools. Treatments are adjusted as necessary if patients are not progressing as expected until the clinical goals are achieved.
- Evidence-Based Care: Patients are offered treatments supported by credible research, ensuring that interventions are effective for their conditions. CoCM is backed by substantial evidence demonstrating its effectiveness, making it one of the most validated integrated care models.
- Accountable Care: Providers are accountable for and reimbursed based on the quality of care and clinical outcomes, rather than the quantity of services provided. This focus on accountability encourages continuous improvement and enhances patient satisfaction.
Enhancing CoCM with CompleteCarePlatform® by kbrax

At kbrax, we have developed the CompleteCarePlatform®, a whole-person centric health platform, designed to support and enhance the Collaborative Care Model. Our platform integrates mental, physical, and social health, providing comprehensive support for patients, providers, and payers.
Key Features of CompleteCarePlatform®
- MindPure Download and Profile Creation: Available as a free download on the Apple iOS App Store and Android Apps on Google Play, MindPure offers users a barrier-free way to engage in meaningful self-monitoring and access resources. The comprehensive MindPure profile captures essential aspects of the patient's health, providing actionable data for personalized care.
- Data Sharing and Self-Monitoring: MindPure facilitates secure, compliant data exchange between users and their care advocates. Patients control their data, sharing it with their care team to foster a collaborative environment focused on their well-being. Interactive check-ins, journaling, and self-monitoring tools help patients track symptoms and share insights with their care team.
- CareCompanion Usage: CareCompanion enhances patient engagement through interactive conversations, capturing a wide range of health data. This comprehensive dataset provides a holistic view of the patient's health, supporting tailored interventions.
- PatientFirst Integration: PatientFirst aggregates data from MindPure, enabling care advocates to gather insights, identify risks, and develop collaborative care plans. This integration ensures that clinical decisions are informed by a holistic view of the patient's health.
- Goal Setting, Reminders, and Measurement: The platform supports goal-setting, monitoring, and reminder functionalities. Patients and care teams establish realistic health goals, with automated reminders to ensure adherence. Progress tracking and regular updates keep patients motivated and informed, leading to better clinical outcomes.
Empowering Patients and Enhancing Care
The CompleteCarePlatform® revolutionizes the care journey by emphasizing a patient-centric, collaborative approach. It supports proactive health management through continuous data collection and real-time insights, allowing timely interventions and adjustments to care plans. Patients are empowered with the tools and information needed to actively participate in their care, resulting in improved health outcomes and a more satisfying care experience.
By integrating MindPure and PatientFirst with the Collaborative Care Model, our platform enhances the quality of care, leading to better health outcomes and a more empowered patient population. Join us on this comprehensive care journey that prioritizes patient-centric, collaborative care, ensuring that healthcare starts and ends with the patient.
